
I volunteered to fight Ebola in Sierra Leone with MSF. Here’s what happened
[Editor’s Note: Please take notice in this story of the fact that MSF asks three questions and warns their doctors before they leave to battle the Ebola virus in Liberia. Interesting that this has NOT gotten the same publicity that the Cuban questions and warnings received – which were, by the way, the same as those asked by MSF…]
I’ve volunteered to go to west Africa because I heard that Médecins Sans Frontières (MSF) was getting desperate for people.
When I tell Mary in HR, she says she has three questions: “1) Do you know that you don’t have to go? 2) Do you know that if you get sick, we won’t bring you home? 3) Do you know that if you die, we won’t bring your body back and you’ll be buried there?” I know MSF is famous for being straight-talking, but I’m still a bit taken aback. I answer yes to all three and go home to look for my passport. My children are unphased – “Yeah, whatever” – but promise to email.
In Brussels, two days later, my medical briefing is entirely in French. It’s a long time since I was at school, but I get the gist: don’t shake hands, rub shoulders or brush fingertips – let alone hug, kiss or have sexual relations – with anyone. In fact, keep 1.5-2 metres away from all people at all times.
Don’t go to markets. Don’t take public transport. And don’t EVER touch your face. By the time I board the plane I have developed a healthy paranoia. And I’m not alone. The cabin crew are wearing face masks, as are many of the passengers. When we touch down in Guinea, another 100 people push their way on. “Ah, it’s Ebola time – everyone is fleeing,” the jovial Liberian beside me says.
Outside Sierra Leone’s Lungi airport, we wash our hands at a barrel with a tap. I learn tap etiquette: after drizzling your hands, you splash water over the tap to rinse off any Ebola germs left by the previous person. This soon becomes a 20-a-day habit – there are taps outside hotels, houses, offices, even the supermarket.

MSF’s newest Ebola treatment centre, 5km outside Bo, is white and gleaming, as incongruous as a spaceship in the surrounding bush. Two months ago it was a field of cassavas – MSF paid the farmer for his crop, then dug up the field and covered it in four enormous white tents, surrounded by brick buildings and divided by orange fencing. I’ve heard Ebola centres described as “villages of death” – six in 10 patients come out in a double body bag – so the atmosphere inside is a surprise. I arrive as three people are given the news that their second test result in a row has showed up negative, and they’re cured.
Excited staff wait outside the concrete shower block, and one by one the survivors emerge, dripping wet and blinking in the sunlight. Everyone claps; James, a pastor turned mental health counsellor, starts to sing, and the others join in; a group of women are dancing; people take photos; everyone beams.

Before they leave, the survivors ask questions. Ishmail: “Will I be able to go near my family now?” Counsellor: “I want you to go home and I want you to hug everyone in your family.” He is given a bag with blankets, bedsheets, multivitamins, packets of peanut paste to build up his strength, and a giant packet of condoms – the virus will survive in his semen for another three months. In the treatment centre, Sierra Leonean staff outnumber the international staff by 10 to one.
All seem enthusiastic about doing their bit. In the kitchen, nine women from the local village are cooking fish and pasta for the patients’ lunch. Alusein, in a Victorian-style mob cap, finds me a pair of white wellies, size 39, decorated with stars and flowers in thick marker pen. In the stock tent, a former philosophy teacher is filling in data sheets. In the mental health tent, James is talking to the family of a patient. “As a pastor, you listen and advise; as a counsellor it’s the same thing,” he says.

I’ve never met people who work so hard. The medics are reprimanded for staying too long inside the high-risk zone. Anything over an hour becomes physiologically dangerous. It’s so hot inside the layers of protective clothing that by the time you come out, you have to pour the sweat out of your boots.
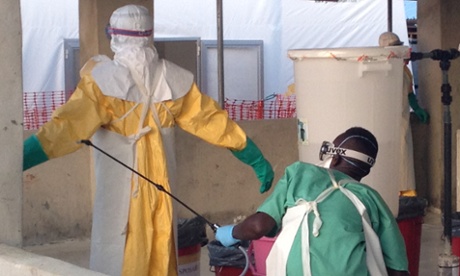
Getting togged up in 10 layers of protective clothing (scrubs, boots, yellow suit, hairnet, hood, mask, goggles, thick gloves, thin gloves, apron), and ensuring that not one millimetre of bare skin is showing, takes time and practice, but it’s nothing compared to undressing.
When you come out of the high-risk zone you are exhausted, overheated and dehydrated; your goggles have misted over, and your mind has gone foggy. There’s a serious risk of getting contaminated as you unzip and unpeel. That’s why the sprayers are there. ”What does your job involve?” I ask. “We are the sprayers, we instruct them what to do, we stop them making mistakes, we save their lives.” They also douse you in 0.5% dilute chlorine – who needs Chanel No 5 when you can smell this sweet?
Everyone here is keen to do anything they can to stop the disease that’s threatening to unravel their whole society – it’s already made travel impossible, put an end to parties and funerals, closed schools and universities, made food prices rocket, and instilled suspicion and fear – of neighbours, friends and even family. “There are no gatherings or naming ceremonies, people are even scared of going to church,” MSF counsellor Tamba says. “They are afraid to do all the things that used to make them happy.”
Mothers no longer want to bring their sick children to MSF’s paediatric hospital in case they get taken away by an alien in a spacesuit and are never seen again. As a result, many of the children only arrive when they are so ill that it’s too late to save them. No one knows how many are dying at home from malaria – the biggest killer of under-fives in this area – or from the numerous other diseases in a country with the highest rate of child deaths in the world.
Hundreds of health workers have caught Ebola and died, there are too few ambulances, too few laboratories, and there’s a very real fear that the entire health system – already weak after years of civil war – is going to collapse.
I monitor my health minutely. Is my headache from dehydration? The sore throat from a chlorine overdose? Am I burning up with fever, or is today hotter than usual? Three symptoms at the same time and you become an Ebola suspect.
My mother emails to suggest my children move into a rented flat in south London for 21 days when I return, while I put myself in self-imposed quarantine. I tell her there is no chance of my infecting anyone, and that I’ll be back in the office the following day. The UK is clearly caught up in Ebola paranoia too. I go out and buy a box of Sierra Leonean chocolates for my work colleagues, and wonder if I’ll get to eat them all myself.
(From the: The Guardian)

